Living longer - please do take this personally
We all respond to our environment in different ways. The same is true of disease and medication. Personalising health care could prevent and treat issues more effectively.
Summary: Early success with an mRNA vaccine for pancreatic cancer points to the emerging importance of precision medicine in extending length of quality life that we enjoy. Precision medicine is one of the categories of personalised medicine recognising that patients are unique, they have different physical, biological and social circumstances and may respond differently to different treatment options.
Why this is important: Whilst there are variations between countries, the world's population is growing and ageing leading to increasing healthcare costs. From an investment perspective, personalised medicine is forecast to be a $1 trillion market by 2028. However developments should result in more effective treatments and preventative measures that increase the overall health of the population with its costs offset by reduced health / social care costs and increased quality of life and productivity.
The big theme: The ongoing survival of the human species is one of the ultimate sustainability themes. Understanding the broad spectrum of influences on human ageing and well-being can help us understand areas for investment as well as individual choices that we can make.

The details
Summary of a study published in Nature:
A small clinical trial of a personalised mRNA-based vaccine against pancreatic ductal adenocarcinoma (PDAC), which accounts for over 90% of pancreatic cancer cases, has demonstrated a strong tumour-specific T-cell response in half of the trial participants, according to results published in Nature. In other words, having been vaccinated, the patient's own immune system identified the cancer as a threat and attacked it. The research, led by Dr Vinod Balachandran from Memorial Sloan Kettering Cancer Center, will now progress to a larger clinical trial. The team used BioNTech, which produced one of the COVID-19 mRNA vaccines, to identify proteins that could trigger an immune response and created a customised mRNA vaccine for each patient, which targeted up to 20 neoantigens (proteins that can be effectively targeted by the immune system).
Pancreatic cancer is one of the most deadly cancers with a survival rate of just 12% that has remained largely unchanged for more than 50 years. It is the 7th leading cause of cancer death globally. Chemotherapy and radiation are not as effective as they are in other cancers with surgery being the main treatment option. Even after surgery, nearly 90% of patients have a recurrence of the disease within 7-9 months. The results from this trial provide some hope.
What is 'mRNA'?
The vaccine in the trial is an mRNA vaccine similar in mode to the COVID19 vaccines produced by Pfizer-BioNTech and Moderna. The same technology is being used to create vaccines for other diseases including respiratory diseases such as influenza. How do they work? what is 'mRNA'?
We introduced some of the structures and mechanisms in the human cell in another Quick Insight. If you are unfamiliar with the basics it's worth a review👇🏾
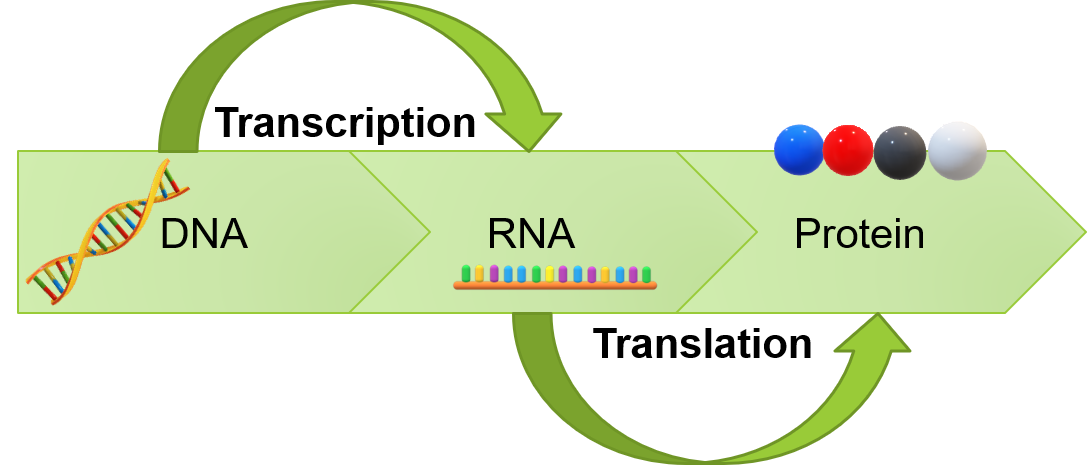
The nucleus or centre of a human cell contains the blueprints / instructions that make us, biologically at least, who we are. These instructions are encoded in our genes which in turn are made of sequences of molecules called DNA. DNA contain information for making specific proteins that ultimately express particular physical characteristics like brown eyes, for example. In order to sustain life, we must continually multiply and replicate our cells, which involves replicating our DNA in addition to using our DNA to create proteins and enzymes that are responsible for gene expression and our overall biological functioning.
The first part of that process of creating proteins is a step call transcription where a piece of DNA that codes for a specific gene is copied into something called 'messenger RNA' or 'mRNA' in the nucleus of the cell. The mRNA then carries that information out of the nucleus into the cytoplasm (the area within the cell surrounding the nucleus) where the information is translated into a protein. And then it's job is done!
The use of mRNA in therapies, such as the vaccines that are targeting PDAC in this trial, involves encoding the mRNA to make a protein that corresponds to the thing you want the immune system to respond to, in this case the patient's individual PDAC tumour. There are a number of challenges that researchers have had to overcome including making the mRNA capable of inducing billions of immune cells by making it more stable. In other words it had to create enough of an immune response to successfully deal with the tumours but not create too much of an immune response that causes other issues.
As well as creating mRNA with the above characteristics, the vaccine was also given the best chance during the trial with all patients receiving a drug called atezolizumab before vaccination, an immune checkpoint inhibitor, which prevents the cancer cells from suppressing the immune system. The patients also started standard chemotherapy drugs for PDAC, once they had been given the vaccine.
Precision and personalised medicine
The vaccine used in the pancreatic cancer clinical trial is an example of precision medicine as the vaccine is designed to work optimally on the specific patient's own tumour. Personalised medicine, which encompasses precision medicine, is one example of a number of broad areas that are being investigated to slow down or even stop biological ageing. It is a topic we have written on previously and will continue to do so 👇🏾

Biological ageing is an important sustainability theme and one which is receiving growing amounts of investment. The payback in terms of saved long term care costs and potentially early diagnosis and treatment could be big, particularly when extrapolated to productivity and quality of life gains. The terms 'personalised medicine' and 'precision medicine' are often used interchangeably but they don't convey exactly the same thing.
Personalised medicine is a holistic approach to healthcare, a broad umbrella that includes other approaches that tailor treatment and preventative measures, of which precision medicine is one type. Precision medicine tends to encompass advanced technologies such as genetic testing, molecular profiling and big data analytics to classify individuals into more precise groups than just age and tailor treatments accordingly. You could say it is about getting the right treatment to the right patient at the right time. Historically if there was a disease X, a treatment Y was found for the disease. If you suffered with X, you were given treatment Y and yes, it may be tailored towards broad age groups, but essentially that was it. Personalised medicine recognises that patients are unique, they have different physical, biological and social circumstances and may respond differently to different treatment options.
How big is the market for personalised medicine? Estimates vary at approximately $500 - $650 billion globally, reaching almost $1 trillion in the next five years. Speaking at a recent conference, the CEO of Juvenescence, a company focused on treating and preventing the underlying causes of age-related diseases, highlighted that in 2022 investments being made into longevity reached $5.2 billion with much of that arguably in precision and personalised medicine.
Examples of personalised medicine
Personalised medicine can treat conditions in a targeted way, but can also help to prevent them by categorising patients in a more granular way. Here are some examples of personalised medicine:
Lifestyle and preventive medicine: Understanding an individual's genetic predispositions and the environmental factors that they are exposed to can enable that individual to avoid doing certain things or doing more of others. Food intolerance tests are good examples here where understanding what foods cause inflammation allow dietary changes to be made. Genetic testing can identify genetic markers associated with increased risks for certain diseases, such as cardiovascular disease and allow for tailored preventive measures such as lifestyle modifications including specific exercise routines, regular screenings, and early interventions.
Pharmacogenomics: A key premise of personalised medicine is that people respond to medications in different ways. Most modern drug development goes through a series of tests or clinical trials to understand how well the drug works, the optimal dosage and what adverse side effects, if any, that there are. Findings from the trials are dependent on the make up of the trial participants. Historically, minority groups, older people and women have been underrepresented in clinical trials. Even putting that to one side, an individual's response can vary with height, weight and many other factors. Within the apparently same group of similar individuals, a drug may be toxic but beneficial, not toxic but beneficial, toxic and not beneficial or have no impact at all. Genetic tests can identify specific variations in a person's genes that may impact their response to certain medications. This information can help doctors select the most effective and safe treatments for individuals, determine the most appropriate drug dosage, minimising adverse reactions and optimising the effectiveness of the treatment.
Targeted therapies: We have already seen the potential with PDAC, and there are other cancer treatments designed to target specific genetic mutations or molecular markers in tumours. Even at a more basic level, greater precision in chemotherapy dosing can reduce adverse side effects and improve the overall outcome.
We shall be discussing this topic as part of a broader discussion in an upcoming Deep Dive 'The death of ageing' that Professional members can read in full.
Something a little more bespoke?
Get in touch if there is a particular topic you would like us to write on. Just for you.
Contact us
Please read: important legal stuff.


