
Hospitals and sustainability
Hospitals and healthcare facilities help sustain human life. But at what cost to the environment?
Summary: There is a growing recognition that health is increasingly affected by climate change, while at the same time global healthcare systems, including inpatient facilities such as hospitals, have a substantial impact on the environment. By looking at factors such as emissions, renewables, logistics, care pathways, supply chains and partnerships, global healthcare has several opportunities to decrease their carbon footprint.
Why this is important: Sustainability themes are interlinked. There will often be trade-offs between them, but that still doesn't mean we can't try to do the best we can in both.
The big theme: Organisations, from individual businesses to industry groupings, are increasingly realising that they are part of broader ecosystems and risks and opportunities need to be seen as interlinked. Regulations and demands from stakeholders are demanding that mindset - double materiality. Understanding the impact of the supply chain will be both demanded but also presents opportunities to improve the sustainability impact of an organisation, regardless of the industry.

The details
Summary of a story from the World Economic Forum
There is an increased awareness of the effects of climate change on global health – negatively affecting the world’s most vulnerable populations – and also on the significant impact healthcare around the world is having on the environment. Healthcare systems are said to account for 4-10% of national CO2 emissions, which is more than the aviation and shipping sectors. As a multi-stakeholder industry that needs high investment to operate, the healthcare sector must start to consider, and be accountable for, their contribution to climate change.
Looking at solutions, there are several strategies that hold potential to bring down the carbon footprint of healthcare. Data is emerging on the possible impact of reducing power consumption, increasing efficiency and turning to renewables; employing sustainable materials and engaging the circular economy; and taking a critical look at supply chains and the efficiency of care. Institutional support and like-minded partnerships will be key in achieving successful implementation of such measures.
Why this is important
Being both affected by and being a contributor to climate change, global healthcare is under increased pressure to scrutinise long-standing practices and procedures across the entire system – from patient care, to data management, to logistics and infrastructure. Hospitals are said to account for up to 10% of a nation’s CO2 emissions, which is not surprising considering hospitals are complex institutions that offer what could be considered one of the widest range of services amongst industries. They are also a large consumer of materials and producer of waste, engaging complex supply chains for both incoming and outgoing operations management. The primary focus of any healthcare system should be the health of communities, and how patients are ‘managed’ – or better said, 'cared for.' Currently, there seems to be a loop of cause and effect on increased use of the system causing increased negative effects on the environment causing increased global health necessitating increased use of the system. A holistic approach to healthcare can mitigate that (subject for a longer blog).
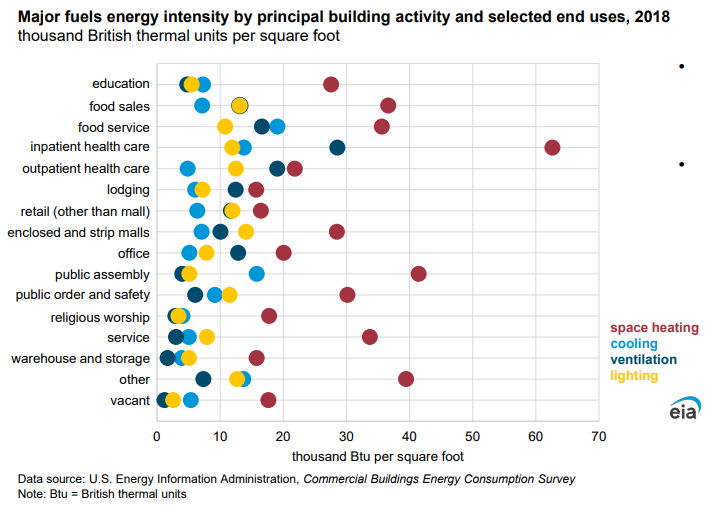
Hospitals by necessity use a lot of power. In 2003, data suggested that inpatient healthcare had the highest energy intensity of all publicly funded buildings in the US and emitted 2.5 times more greenhouse gases than commercial buildings. The latest Commercial Buildings Energy Consumption Survey (CBECS) however showed a 16% decrease in energy intensity for inpatient healthcare between 2012 and 2018, although they still had the highest energy intensity for both space heating and ventilation as well as one of the highest for lighting. However, a simple solution of ‘turning off the lights’ may not always be a viable option in settings that run on 24-hours power needs like hospitals. Therefore a focus on lower emission energy sources, including switching to renewable and more efficient power sources, can have an impact. Boston Medical Centre (BMC), for example, generates much of its own electricity and heat through a 2MW combined heat and power plant installation. In 2016 it entered into a purchase agreement with MIT and the Post Office Square Redevelopment Corporation committing to buy 26% of the power generated from a proposed 60MW solar installation (which went on line in 2017). That is the equivalent of all of BMC's projected electricity consumption.
Another area is medical equipment energy use and opting for more efficient equipment, such as eco-designed imaging equipment (unsurprisingly detailed in the WEF article given that it was authored by the head of sustainability at Philips). COCIR, which is the European Trade Association representing the medical imaging, radiotherapy, health ICT and electromedical industries, has a voluntary industry initiative to improve the energy and material efficiency of medical imaging equipment.
Increased use of alternative and more sustainable materials, reuse and waste reduction could all help in reducing healthcare systems’ footprint, as well as increasing budget efficiency in an industry under constant and increasing financial pressure. For example, anaesthetic gases most commonly used including nitrous oxide and fluorinated gases have global warming potentials (100 years) between 130 kgCO2e/kg and 2,540 kgCO2e/kg. Some estimates suggest anaesthetic gases contribute to 0.6% of hospital emissions globally but arguably the data is incomplete. Having said that reducing the need for surgery and anaesthetic is incrementally worthwhile. For example, surgical debridement (removal of dead tissue from a wound) could be replaced by more... ahem... natural methods. Sometimes even simple behavioural changes can have a big impact. Nurses at Great Ormond Street Hospital in London noted that staff were using non-surgical gloves instead of washing hands when bathing babies or moving beds. Through re-education the hospital was able to cut its use of plastic gloves saving £90,000 and 21 tonnes of plastic.
Digitisation of services, information management and, even virtualisation of care, is also at the forefront of how healthcare systems can decrease usage of facilities and in turn emissions. Online care hubs may increase patient engagement by increasing ease of accessibility. It may also improve the efficiency of the patient journey, one which often includes several visits between diagnosis, treatment, monitoring and follow up. Furthermore, a decrease in CO2 emissions by engaging online resources rather than necessitating travel and in-person visits cannot be ignored.
Finally, hospitals and other inpatient care facilities do not function on their own, and demanding better accountability from all participants in the supply chain is essential for change. The supply chain accounts for 71% of CO2 emissions within the EU according to a report by Healthcare without harm and construction firm Arup, with the "vast majority of [those] emissions emanat[ing] from the production, packaging, transport, and disposal of goods and services that health care purchases." Decreasing the impact of healthcare means taking an end-to-end view of the value chain, making procurement a central component of sustainability efforts. With the SEC Climate Disclosure rules likely to come into effect from April of 2023, that focus on understanding emissions through the supply chain will become a requirement regardless of the industry.
(The pharmaceutical industry is a big sustainability topic in its own right, environmentally, socially and from a governance perspective. It is of course an important part of the health care supply chain. We shall discuss in a more detailed blog)
Something a little more bespoke?
Get in touch if there is a particular topic you would like us to write on. Just for you.
Contact us
Please read: important legal stuff.

